| When does the pursuit of ‘best practices’ make sense, and when do we need to apply less precise but more effective approaches instead?
What Surowiecki seems to be looking for is what in business is called ‘best practices’. What’s interesting to me is that business has recently become disenchanted with ‘best practices’: In a world where every job, every situation, every context is different, the applicability of some documented ‘best practice’ in any situation other than the one it was identified in is increasingly dubious. Dave Snowden articulates these three ‘heuristics’ about real-world knowledge: Knowledge can only be volunteered; it can’t be conscripted.
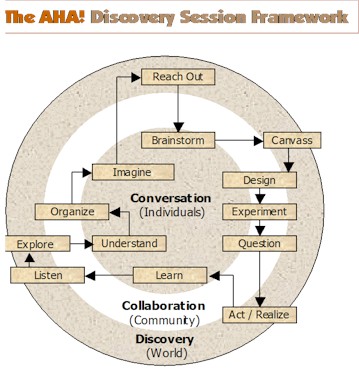
People always know more than they can tell and can tell more than they can write. People only know what they know when they need to know it. Human knowledge is contextual and triggered by circumstance. So what we have here is a clash of two new and exciting philosophies: Surowiecki’s argument that tapping the Wisdom of Crowds can allow much better answers to emerge than relying on experts, versus Snowden’s argument that such ‘wisdom’ is possible and useful only in relatively simple situations where apples can clearly be compared to apples, and doesn’t work in the majority of more complex situations where every case is arguably significantly different. An identified ‘problem’ in Surowiecki’s article is the large number of facilities and practitioners providing over-long stays to patients in Florida, compared to other states. They are drawn there, of course, because that’s where the customers are, and, as in all things, the work tends to expand to fill the available space, money and time. In public health services we seem to try to offset these ‘market’ tendencies by making sure both facilities and practitioners’ time are in constant short supply, in the presumption that this will yield less waste and force greater efficiency, rather than posing a serious threat to public health. And this is exactly the problem with applying mechanistic, industrial, simple-situation prescriptions to complex-situation challenges. So what should we do when doctors in one community perform appendectomies and tonsillectomies four times as often as they do in the next community, of the same size, a stone’s throw away? Surowiecki thinks we need to figure out “how to pay doctors for the quality, rather than the quantity, of the care they provide” and hopes that “eventually people will start paying attention to the data and recognize how costly these variations can be”. But even he seems dubious of the possibility of either of these things happening. Of course patients need to be better informed about preventative health care, self-treatment and new knowledge about less invasive and unnecessary procedures. But health care isn’t like widgets, where differences in ‘unit’ product cost, quality and service are conspicuous. Every situation is truly different, and we’ll never come up with either a formula for determining the right health care answer, or an expert system that will tell us precisely where the ‘inefficiencies’ in health care are and how they can be eliminated. Surowiecki suggests the problem is geography and parochialism. But geography is just one way of slicing community, and these days it’s not even the most important one. The issue isn’t isolation of community, it’s incomparability of situations with infinitely many different contexts. When the data is a million cases of one, the significance of patterns is likely to be illusory. And health care isn’t the exception either — most of the products and services that are essential to human well-being, like education, nutrition, freedom, justice, security, transparency of government and a healthy environment are also enormously contextual, circumstantial and relative. Experts and advocates in these fields have torn out their hair trying to find benchmarks, standards, measures, scorecards and ‘best practices’ that will allow us to cajole improvements in performance from those we assess to be falling short. It can’t be done. Complicated solutions don’t solve complex problems. The essence of Snowden’s new approach to sense-making and management ‘science’ is to first assess whether the situation lends itself to simple-to-complicated solutions and approaches (like root cause analysis, systems thinking and The Wisdom of Crowds), or if it requires more complex approaches (like cultural anthropology, pattern-seeking, Open Space and emergent understanding techniques like the AHA! Discovery Framework diagrammed above). It doesn’t take much thought to realize (a) that most of the challenges we face in business and society today are complex, and (b) attempts to force simple and complicated-situation solutions in complex situations, like the deliberate starving of the health and education systems (and like the ubiquitous imposition of lousy service in all areas of business today), in the ill-conceived belief these will somehow mechanically force efficiency and productivity improvements in them, are doomed to make the situations worse, not better. It’s time we woke up to the realization that industrial-age solutions are increasingly inapplicable in the information age, and it’s time we got over our discomfort with the imprecision, uncertainty, lack of causality, and non-amenability to command-and-control hierarchy that complex approaches entail. Managers, grit your teeth and prepare for some revolutionary new, difficult and important learning. So sorry, health care fans desperate for solutions to spiraling costs. No ‘best practices’ or ‘popular wisdom’ answers here. Move along, please. |
Navigation
Collapsniks
Albert Bates (US)
Andrew Nikiforuk (CA)
Brutus (US)
Carolyn Baker (US)*
Catherine Ingram (US)
Chris Hedges (US)
Dahr Jamail (US)
Dean Spillane-Walker (US)*
Derrick Jensen (US)
Dougald & Paul (IE/SE)*
Erik Michaels (US)
Gail Tverberg (US)
Guy McPherson (US)
Honest Sorcerer
Janaia & Robin (US)*
Jem Bendell (UK)
Mari Werner
Michael Dowd (US)*
Nate Hagens (US)
Paul Heft (US)*
Post Carbon Inst. (US)
Resilience (US)
Richard Heinberg (US)
Robert Jensen (US)
Roy Scranton (US)
Sam Mitchell (US)
Tim Morgan (UK)
Tim Watkins (UK)
Umair Haque (UK)
William Rees (CA)
XrayMike (AU)
Radical Non-Duality
Tony Parsons
Jim Newman
Tim Cliss
Andreas Müller
Kenneth Madden
Emerson Lim
Nancy Neithercut
Rosemarijn Roes
Frank McCaughey
Clare Cherikoff
Ere Parek, Izzy Cloke, Zabi AmaniEssential Reading
Archive by Category
My Bio, Contact Info, Signature Posts
About the Author (2023)
My Circles
E-mail me
--- My Best 200 Posts, 2003-22 by category, from newest to oldest ---
Collapse Watch:
Hope — On the Balance of Probabilities
The Caste War for the Dregs
Recuperation, Accommodation, Resilience
How Do We Teach the Critical Skills
Collapse Not Apocalypse
Effective Activism
'Making Sense of the World' Reading List
Notes From the Rising Dark
What is Exponential Decay
Collapse: Slowly Then Suddenly
Slouching Towards Bethlehem
Making Sense of Who We Are
What Would Net-Zero Emissions Look Like?
Post Collapse with Michael Dowd (video)
Why Economic Collapse Will Precede Climate Collapse
Being Adaptable: A Reminder List
A Culture of Fear
What Will It Take?
A Future Without Us
Dean Walker Interview (video)
The Mushroom at the End of the World
What Would It Take To Live Sustainably?
The New Political Map (Poster)
Beyond Belief
Complexity and Collapse
Requiem for a Species
Civilization Disease
What a Desolated Earth Looks Like
If We Had a Better Story...
Giving Up on Environmentalism
The Hard Part is Finding People Who Care
Going Vegan
The Dark & Gathering Sameness of the World
The End of Philosophy
A Short History of Progress
The Boiling Frog
Our Culture / Ourselves:
A CoVid-19 Recap
What It Means to be Human
A Culture Built on Wrong Models
Understanding Conservatives
Our Unique Capacity for Hatred
Not Meant to Govern Each Other
The Humanist Trap
Credulous
Amazing What People Get Used To
My Reluctant Misanthropy
The Dawn of Everything
Species Shame
Why Misinformation Doesn't Work
The Lab-Leak Hypothesis
The Right to Die
CoVid-19: Go for Zero
Pollard's Laws
On Caste
The Process of Self-Organization
The Tragic Spread of Misinformation
A Better Way to Work
The Needs of the Moment
Ask Yourself This
What to Believe Now?
Rogue Primate
Conversation & Silence
The Language of Our Eyes
True Story
May I Ask a Question?
Cultural Acedia: When We Can No Longer Care
Useless Advice
Several Short Sentences About Learning
Why I Don't Want to Hear Your Story
A Harvest of Myths
The Qualities of a Great Story
The Trouble With Stories
A Model of Identity & Community
Not Ready to Do What's Needed
A Culture of Dependence
So What's Next
Ten Things to Do When You're Feeling Hopeless
No Use to the World Broken
Living in Another World
Does Language Restrict What We Can Think?
The Value of Conversation Manifesto Nobody Knows Anything
If I Only Had 37 Days
The Only Life We Know
A Long Way Down
No Noble Savages
Figments of Reality
Too Far Ahead
Learning From Nature
The Rogue Animal
How the World Really Works:
Making Sense of Scents
An Age of Wonder
The Truth About Ukraine
Navigating Complexity
The Supply Chain Problem
The Promise of Dialogue
Too Dumb to Take Care of Ourselves
Extinction Capitalism
Homeless
Republicans Slide Into Fascism
All the Things I Was Wrong About
Several Short Sentences About Sharks
How Change Happens
What's the Best Possible Outcome?
The Perpetual Growth Machine
We Make Zero
How Long We've Been Around (graphic)
If You Wanted to Sabotage the Elections
Collective Intelligence & Complexity
Ten Things I Wish I'd Learned Earlier
The Problem With Systems
Against Hope (Video)
The Admission of Necessary Ignorance
Several Short Sentences About Jellyfish
Loren Eiseley, in Verse
A Synopsis of 'Finding the Sweet Spot'
Learning from Indigenous Cultures
The Gift Economy
The Job of the Media
The Wal-Mart Dilemma
The Illusion of the Separate Self, and Free Will:
No Free Will, No Freedom
The Other Side of 'No Me'
This Body Takes Me For a Walk
The Only One Who Really Knew Me
No Free Will — Fightin' Words
The Paradox of the Self
A Radical Non-Duality FAQ
What We Think We Know
Bark Bark Bark Bark Bark Bark Bark
Healing From Ourselves
The Entanglement Hypothesis
Nothing Needs to Happen
Nothing to Say About This
What I Wanted to Believe
A Continuous Reassemblage of Meaning
No Choice But to Misbehave
What's Apparently Happening
A Different Kind of Animal
Happy Now?
This Creature
Did Early Humans Have Selves?
Nothing On Offer Here
Even Simpler and More Hopeless Than That
Glimpses
How Our Bodies Sense the World
Fragments
What Happens in Vagus
We Have No Choice
Never Comfortable in the Skin of Self
Letting Go of the Story of Me
All There Is, Is This
A Theory of No Mind
Creative Works:
Mindful Wanderings (Reflections) (Archive)
A Prayer to No One
Frogs' Hollow (Short Story)
We Do What We Do (Poem)
Negative Assertions (Poem)
Reminder (Short Story)
A Canadian Sorry (Satire)
Under No Illusions (Short Story)
The Ever-Stranger (Poem)
The Fortune Teller (Short Story)
Non-Duality Dude (Play)
Your Self: An Owner's Manual (Satire)
All the Things I Thought I Knew (Short Story)
On the Shoulders of Giants (Short Story)
Improv (Poem)
Calling the Cage Freedom (Short Story)
Rune (Poem)
Only This (Poem)
The Other Extinction (Short Story)
Invisible (Poem)
Disruption (Short Story)
A Thought-Less Experiment (Poem)
Speaking Grosbeak (Short Story)
The Only Way There (Short Story)
The Wild Man (Short Story)
Flywheel (Short Story)
The Opposite of Presence (Satire)
How to Make Love Last (Poem)
The Horses' Bodies (Poem)
Enough (Lament)
Distracted (Short Story)
Worse, Still (Poem)
Conjurer (Satire)
A Conversation (Short Story)
Farewell to Albion (Poem)
My Other Sites

 This week’s New Yorker has another interesting column by James Surowiecki, entitled
This week’s New Yorker has another interesting column by James Surowiecki, entitled 

Geez, first glance at your post and my hackles immediately went up. Reading, I was calculating how much effort needed to be expended in answering. Then, your intent was revealed. Good thing, too; I like believing you to be aware.
The problem with “best practices” is, they’re determined by ass-brained bosses who know more about organizational/management culture industry-wide than they do about the actual production process within their own organization. I work in a hospital, and I don’t know how many times I’ve got an official happy-talk handout from HR about some new policy, justifying it as the “industry trend” or because “x out of y” hospitals in the region were already doing it that way. But since, as Kenneth Boulding observed, large hierarchical organizations create imaginary worlds in the minds of those at the top, their only feedback on how these “best practices” work out comes from those at the top of other organizations: resume carpet-baggers who have been shuffling between senior management jobs in one organization after another, who are just as clueless as they are. The only people in a position to identify the “best practices” in an organization are those at the bottom doing the actual work. And the bosses care fuck-all what we have to say. In fact, many corporations are so large that the transaction costs of identifying “best practices” and relaying the information to those in a position to implement them are higher than any possible savings. The only thing that keeps such organizations going is that they all belong to the same oligopoly industry, each firm competing against others with organizational cultures just as pathological as their own.
Just fyi .. in your neck of the woods (toronto) Cindy gordon and her helix commerce offering have just recently entered into strategic alliance with david Snowden and the Cynefin (Centre/Institute ?) to offer capabilities in “managing complexity”.I imagine that you know Cindy from your respective involvements in KM, but if not and you wantto connect with her, mike mcinerney knows her well and would introduce, I am sure.Personally, i’m dubious, as the material I received in an email brochure reads distressingly like all the other promises of consulting solutions-oriented fare … which means sell something that won’t go deep enough and won’t address rigorously enough the really hard mental-model and dynamics changing work that your “discomfort with the imprecision, uncertainty, lack of causality, and non-amenability to command-and-control hierarchy that complex approaches entail” statement sets out as a critical challenge.
It’s unfortunate but understandable that this short New Yorker piece only looked at one part of the work of Wennberg and colleagues (with whom I have worked, in communications, for over a decade). As you so rightly point out here, Dave, and Kevin complains, change based on “best practices” alone doesn’t work, especially when it alienates and disregards the people who actually deliver the care. Wennberg’s group, and others, are looking not only at policy and organizational issues (and I’d argue that this is very important; without the patterns that these sorts of studies reveal it would be all too easy to ignore the incredible discrepancies that exist) but at strategies for empowering people at the microsystem level (the family-practice clinic, the intensive care unit) to study their own system and work together to create greater efficiency, quality, and team/patient satisfaction rather than having a top-down system “imposed”. They are also providing and encouraging graduate-level and medical school training to teach these concepts and hopefully help both new health care providers and mid-career professionals from experiencing the incredible frustration and burn-out we now see in the system. Only by creating a way for administrators, policy-makers, providers, staff and patients to understand the dynamics of this complex system and communicate together will we end up with any hope of real change – especially change that benefits the patient.